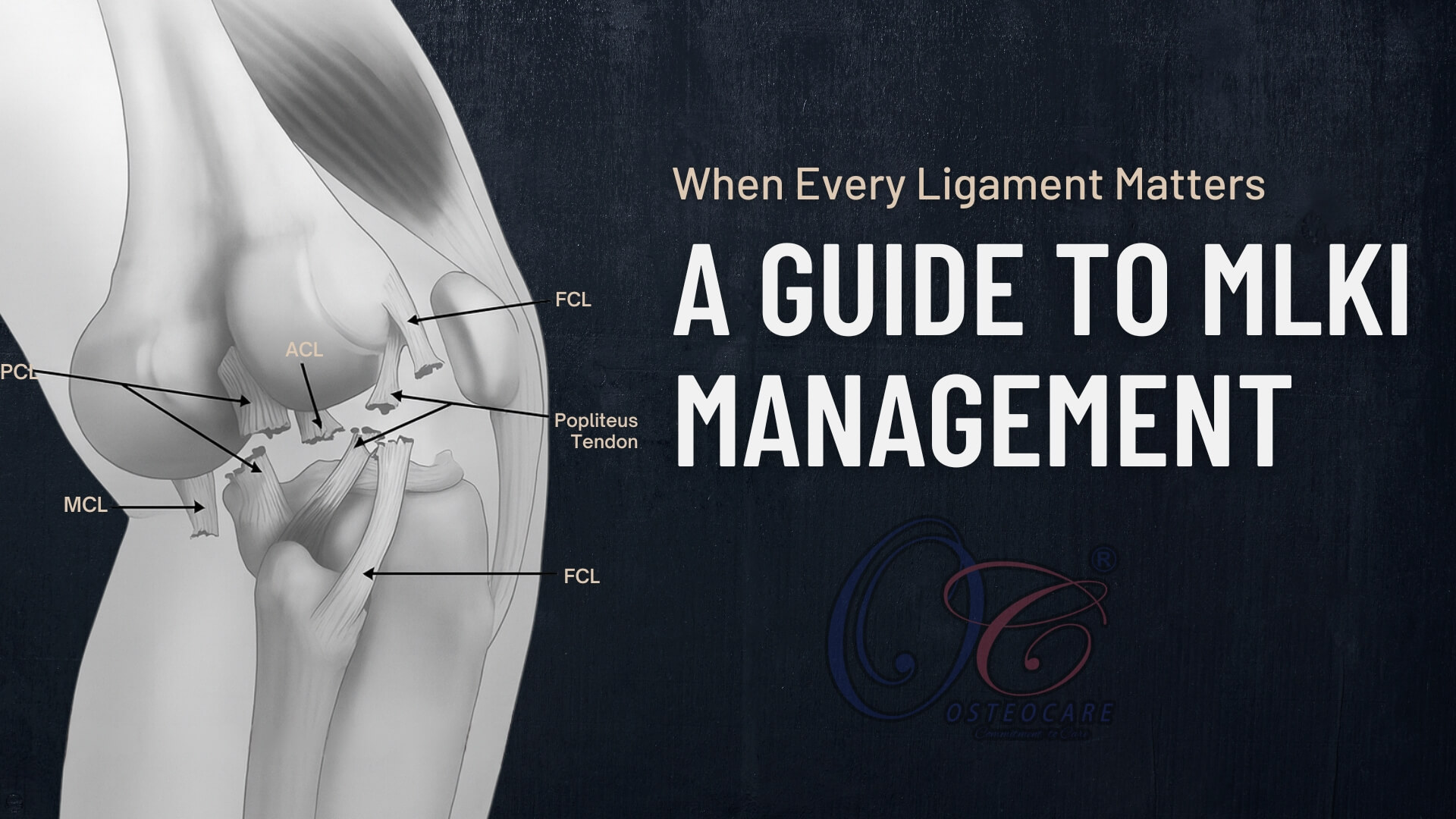
Multiligament Knee Injuries (MLKIs) are complex, often high-energy injuries involving two or more of the four major knee ligaments: the Anterior cruciate ligament (ACL), the Posterior cruciate ligament (PCL), the Medial collateral ligament (MCL), and the Lateral collateral ligament/Posterolateral corner (LCL/PLC). These injuries result in significant joint instability and represent a serious challenge in orthopedic trauma, often leading to poor functional outcomes and long-term arthritis if not managed appropriately.
Classifying Multiligament Injuries
Multiligament injuries are most commonly classified by using the Schenck classification system for knee dislocation (KD). This system categorizes the injury based on the direction of tibial displacement relative to the femur.
Schenck’s classification system for knee dislocation (KD).
| Classification | Description | Injured structures |
|---|---|---|
| KD-I | Isolated ligament injury | ACL or PCL |
| KD-II | Bicruciate ligament injury | ACL and PCL |
| KD-III-M | Bicruciate injury with medial-sided disruption | ACL, PCL, and MCL |
| KD-III-L | Bicruciate injury with lateral-sided disruption | ACL, PCL, and FCL |
| KD-IV | Dislocation with periarticular fracture | ACL, PCL, MCL, FCL, and periarticular bones |
| KD-V | Bicruciate injury with lateral-sided disruption | ACL, PCL, and FCL |
ACL: Anterior cruciate ligament, PCL: Posterior cruciate ligament, MCL: Medial collateral ligament, FCL: Fibular collateral ligament, M: Medial, L: Lateral
🔎 Assessment of MLKIs
A thorough and systematic assessment is critical due to the potential for limb-threatening vascular inury and associated nerve damage.
| Assessment Phase | Component | Key Actions & Tests | Rationale & Significance |
|---|---|---|---|
| 1. Primary Survey (Limb-Threatening) | Neurovascular Status | Immediate priority. Assess before detailed ligamentous exam. | To rule out vascular injury or compartment syndrome, which are surgical emergencies. |
| Vascular Assessment |
|
|
|
| Neurological Assessment |
|
The peroneal nerve is the most commonly injured nerve, especially with PLC injuries. | |
| 2. Secondary Survey (Structural) | Physical Examination | Performed when limb is stable; exam under anesthesia may be required. | Used to classify injury pattern (KD-I to KD-V). |
| Ligamentous Stability Tests |
|
|
|
| 3. Diagnostic Confirmation & Planning | Imaging | Essential for diagnosis and surgical planning. | |
| Plain Radiography |
|
Rules out fractures and identifies dislocation type. | |
| Stress Radiography |
|
Measures joint line gapping to grade collateral ligament injuries. | |
| MRI |
|
Identifies ligament tears, cartilage injury, meniscal tears, bone bruising. |
Surgical Reconstruction
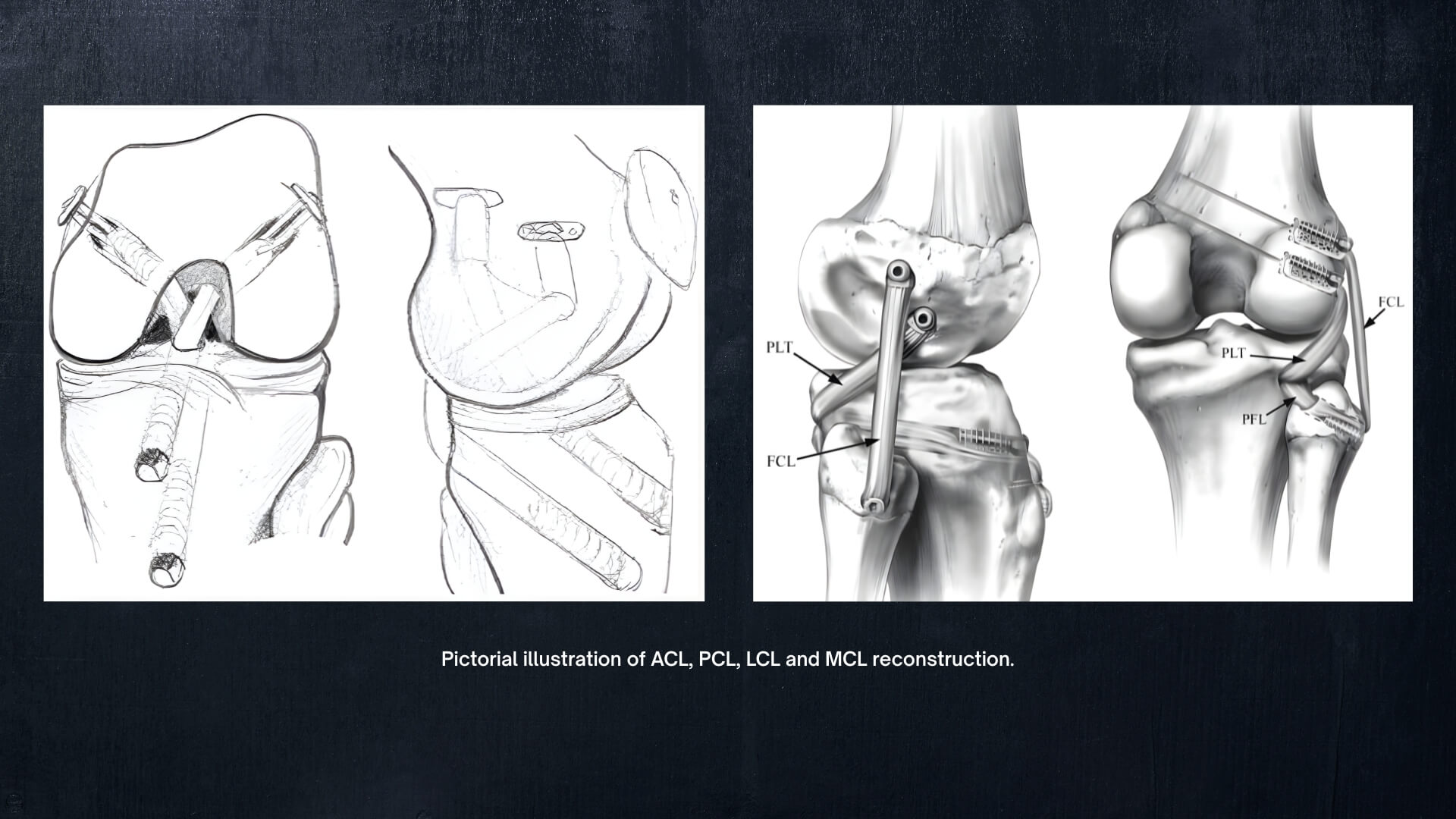
The surgical approach is tailored to the specific injury pattern (KD type). The general principle is to reconstruct the cruciate ligaments (ACL/PCL) first to restore central stability, followed by the collateral ligaments/PLC.
- ACL/PCL Reconstruction: These are typically performed anatomically, drilling tunnels through the femur and tibia.
- Collateral Ligaments: The MCL is often repaired or reconstructed. The PLC is generally reconstructed with two separate tendon bundles (e.g., FCL and Popliteus) to recreate its complex anatomy.
Most MLKIs are addressed in a single-stage surgery, where all damaged ligaments are reconstructed in one operation. However, in some cases with severe bony fractures or irreparable vascular injuries, a staged surgery may be necessary, addressing the most critical issues first and the ligaments later.
Avoiding Tunnel Convergence
A critical technical challenge is Avoiding Tunnel Convergence. This occurs when multiple drill tunnels (for ACL, PCL, and sometimes collateral ligaments) cross or compromise each other within the femur or tibia, which can lead to inadequate fixation or tunnel enlargement.
- Strategies to Avoid Convergence:
-
- Staging the surgery: Performing ACL/PCL first, then addressing the collaterals.
- Using different portals/angles: Adjusting the entry points and angles for the drill guides to maximize bone bridges between tunnels.
- Anatomic Placement: Precise, anatomic tunnel placement is the best defence against convergence.
- Femoral Fixation: Using independent suspension devices (e.g., buttons) instead of cross-pin fixation near the femoral tunnels can save space.
The Recovery Timeline: A Phased Approach
| Phase | Timeline | Key Goals | The “Do Not” List |
|---|---|---|---|
| Phase 1: Protection | Weeks 0–6 |
|
|
| Phase 2: Motion | Weeks 6–12 |
|
|
| Phase 3: Strength | Months 3–9 |
|
|
| Phase 4: Return | Months 9–18+ |
|
|
Conclusion
Multiligament knee injuries represent a complex challenge requiring a team-based approach. Advances in imaging, surgical techniques, fixation innovations, and structured rehabilitation have transformed the way surgeons treat MLKIs today. With precise diagnosis, meticulous reconstruction, and dedicated rehabilitation, patients can achieve stable, functional knees and often return to their previous level of activity.
